Contributor: Ja’Davia Schafer, M.S., PCOM Georgia D.O. Candidate Class of 2023
RM with type 2 diabetes, arthritis and heart condition recently inquired about whether a fish oil supplement would be beneficial for her. She is currently taking insulin degludec, empagliflozin and semaglutide for her diabetes as well as rosuvastatin for her cholesterol. Would a fish oil supplement or prescription product be appropriate for RM?
According to the 2010 Dietary Guidelines reported by the National Center for Complementary and Integrative Health (NCCIH), it was recommended that individuals consume a variety of 8 ounces of fish or more per week due to the variety of nutrients provided (1). Many individuals supplement this with a dosage of 250–500 mg over-the-counter fish oil pills per day (2). This is the recommended dosage for the average healthy adult in the United States, however, they should not serve as a full replacement of whole foods.
These translucent yellow supplements contain Polyunsaturated fatty acids (PUFA). One key subgroup of PUFA is omega-3 fats including, Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which is found primarily in fish and fish oils (3). Extensive research studies have shown that diets high in EPA and DHA have significantly lowered the risk of heart and other inflammatory diseases (4). Diets high in PUFA and monounsaturated, such as the Mediterranian diet, have shown to reduce the instances of coronary artery disease, ischemic strokes, and lowering cholesterol (5, 6). Individuals with pre-existing heart conditions also benefit from taking OTC fish oil supplements, however, these patients have better outcomes from taking prescription medications such as statins (HMG CoA reductase inhibitor that reduces the production of cholesterol) or prescription omega-3 PUFA formalations (7). (an FDA approved ethyl esters of omega-3 fatty acids that contain a higher amount of DHA and EPA). The FDA approved prescription omega-3 PUFA formulations are indicated for treatment of triglyceride levels of 500 mg/dL or greater.
- LovazaⓇ (omega-3 acid ethyl ester of EPA/DHA)
- EpanovaⓇ (omega-3 carboxylic acid of EPA/DHA)
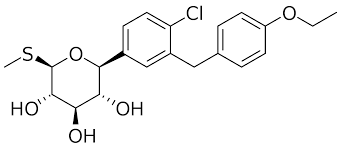
- VascepaⓇ (ethyl ester of EPA only)
The amount of EPA/DHA per capsule is 1 gram in the prescription omega-3 PUFA formulations and less than 300 mg per capsule OTC fish oil supplements (8). For prescription formulations, the total daily dose is 2 – 4 grams. Typically an OTC fish oil supplement can be purchased for less than $10 (Look for the buy one get one FREE deals.) while the prescription fish oil products will be at least $40 without insurance coverage. In terms of side effects, some people may notice a “fishy” taste, dyspepsia (with LovazaⓇ) or increased risk of bleeding event (VascepaⓇ) (so be cautious if you have a history of bleeding event).
Questions you should ask during your provider visit regarding fish oil:
- Can I take a fish oil supplement or prescription product considering all of my current health conditions?
- Can I take a fish oil supplement or prescription product with my other medication?
- Do I need to separate when I take fish oil from my other medications?
- Would a fish oil supplement or prescription product be better for me?
- Can I take these supplements while pregnant?
- What are some signs that I may be deficient in omega 3 fatty acids?
Back to RM, after collaborating in the decision making process, a prescription fish oil product was selected. RM followed up in a week sharing that she has tolerated it without any side effects.
References:
1. 7 Things to Know About Omega-3 Fatty Acids. National Center for Integrative Health.
https://www.nccih.nih.gov/health/tips/things-to-know-about-omega-fatty-acids#pdf. Accessed on February 20, 2021.
2. Interim Summary of Conclusions and Dietary Recommendations on Total Fat & Fatty Acids. The Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in Human Nutrition. Nov 2008. https://www.who.int/nutrition/topics/FFA_summary_rec_conclusion.pdf?ua=1. Accessed on February 20, 2021.
3. PM Kris-Etherton, Denise Shaffer Taylor, Shaomei Yu-Poth, Peter Huth, Kristin Moriarty, Valerie Fishell, Rebecca L Hargrove, Guixiang Zhao, Terry D Etherton. Polyunsaturated fatty acids in the food chain in the United States. The American Journal of Clinical Nutrition, Volume 71, Issue 1, January 2000, Pages 179S–188S, https://doi.org/10.1093/ajcn/71.1.179S
4. H Gerster. Can adults adequately convert alpha-linolenic acid (18:3n-3) to eicosapentaenoic acid (20:5n-3) and docosahexaenoic acid (22:6n-3). Int J Vitam Nutr Res. 1998;68(3):159-73.
5. Why the Mediterranean Diet is Good for your Heart. Harvard Women’s Health Watch. https://www.health.harvard.edu/heart-health/why-the-mediterranean-diet-is-so-good-for-your-heart. Accessed on February 20, 2021.
6. Miguel A. Martínez-González, Alfredo Gea, Miguel Ruiz-Canela. The Mediterranean Diet and Cardiovascular Health. Circulation Research. 2019;124:779–798. https://doi.org/10.1161/CIRCRESAHA.118.313348
7.L DeDea. When to take statins; Lovaza versus OTC Fish Oil Supplements. Journal of the American Academy of PAs. 2001;24(5):23.
8. MS Kelly, C Beavers, JD Bucheit, et al. Pharmacologic approaches for the management of patients with moderately elevated triglycerides (150 – 499 mg/dL). J Clin Lipidol, 2017;11:872-879.